Sjogren’s Syndrome
Clinical features
– Dry eyes (keratoconjunctivitis sicca): initially asymptomatic, later gritty sensation, itching, soreness or inability to cry.
– Salivary and lacrimal glands may swell.
– Dry mouth (xerostomia): difficulty in eating dry foods, disturbed taste,
speech and swallowing, rampant caries, candidosis and acute sialadenitis.
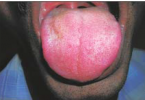
– Saliva is frothy and not pooling; parchment-like mucosa and lobulated depapillated tongue.
– There is no connective tissue disease in primary Sjögren’s syndrome, but it is present
in secondary: typically rheumatoid arthritis or primary biliary cirrhosis, and occasionally other autoimmune disorders.
– A similar syndrome may be seen in HIV disease.
Incidence
– Uncommon: mainly middle-aged or elderly women.
Aetiology
– Autoimmune inflammatory exocrinopathy. There may be a viral aetiology and a
genetic predisposition.
Diagnosis
– Clinical. Ro (SS-A), La (SS-B) and other autoantibodies, especially rheumatoid factor.
– Salivary flow rates reduced.
– Labial gland biopsy, sialography and/or scintigraphy or ultrasonography.
– Differentiate from other causes of xerostomia, especially drugs (anticholinergics such as
tricyclic antidepressants and sympathomimetics), dehydration, HIV salivary gland disease, irradiation, sarcoidosis.
Management
– Control underlying disease: at present experimental (e.g. ciclosporin).
– Eyes – methylcellulose eye drops or rarely ligation or cautery of nasolacrimal duct.
– Dry mouth – preventive dental care (oral hygiene, limitation of sucrose intake, fluorides, chlorhexidine, xylitol-containing chewing gum) Treat infections.
– Sialogogues and/or salivary substitutes (e.g. methylcellulose). Pilocarpine, cevimeline or bethanechol may be used to stimulate salivation.


ــــــــــــــــــــ► ⒹⒺⓃⓉⒶⓁ–ⓈⒸⒾⒺⓝⓒⒺ ◄ــــــــــــــــــــ