Factors Influencing the Success of Root Coverage Procedures
1. Patient Characteristics
– Gingival recession is often a source of anxiety to patients.
– Noncompliant patients should be considered at risk.
– It was suggested that the clinician should carefully assess patient‘s expectations and
motivation for seeking treatment.
– An unsatisfied patient already subjected to multiple aesthetic procedures should be
suspected of never being satisfied.
– The demand for repeated surgery can be, in fact, a sign of psychopathology
(polysurgical addiction).
– Patients presenting factitious gingival ulceration should be carefully evaluated prior to root coverage procedures.
– Patients with poor oral hygiene who are prone to periodontal destruction are also at great risk for surgical failure unless the local factors can be controlled.
– In addition to clinical outcomes, another aspect to be considered is the possible change in the soft tissues caused by smoking.
– A recent meta-analysis performed by Chambrone et al. indicated a statistically significant greater reduction in gingival recession (P <0.001) and gain in clinical attachment level
(P < 0.001) for nonsmokers when compared with smokers whose gingival recession was treated with subepithelial connective-tissue grafts.
– Additionally, nonsmokers exhibited significantly more sites with complete root coverage than did smokers (P = 0.001). Subepithelial connective-tissue grafts resulted in 27.0 to 80.0% complete root coverage for nonsmokers and 0 to 25.0% for smokers.
– Similarly, coronally advanced flaps resulted in 20.0 to 55.1% complete root cov erage for
nonsmokers and 0 to 54.5% for smokers. For guided tissue regeneration, complete root coverage was 38.5% for nonsmokers and 11.1% for smokers. Between smokers and
nonsmokers who received subepithelial connective-tissue grafts, nonsmokers achieved more complete root coverage.
– They showed a significant difference in the number of sites with complete root coverage when compared with smokers (risk ratio, 0.24; 95% CI: 0.10 to 0.58) in the two arms of the trials.
– Similar results were revealed by Souza et al. (2008) who showed that smoking can reduce
the root coverage obtained with an SCTG associated with a coronally positioned flap.
– The percentages of root coverage in smokers after 3 months (62.10% ± 19.08%) and 6 months (58.02% ± 19.75%) were substantially lower than that of non-smokers (82.17% ± 16.47% and 83.35% ± 18.53%, respectively).
2. Anatomic Features
– In the literature, gingival recessions have been classified into four classes, according to the prognosis of root coverage.
– In Class I and II gingival recessions, there is no loss of interproximal periodontal attachment and bone and complete root coverage can be achieved; in Class III, the loss of interdental periodontal support is mild to moderate, and partial root coverage can be accomplished; in Class IV, the loss of interproximal periodontal attachment is so severe that no root coverage is feasible.
– More recently, other factors than the level of interproximal attachment and bone have been shown to limit the amount of root coverage: the reduction of papilla height, tooth rotation and tooth extrusion with or without occlusal abrasion.
– In all these clinical situation, only partial root coverage can be achieved.
– The smile line also needs to be considered. Normally, the cosmetic zone is limited to the
maxilla.
– Patients presenting a gummy smile should be carefully evaluated before root coverage
procedures.
– The surgical challenge is great, because the smile will expose the entire operated zone.
– These patients may require orthodontics and orthognatic surgery to improve the lip line.
3. Technique Characteristics
– Periodontal plastic surgery is an art as much as an science and a skilled practitioner can
obtain more satisfactory results than those with less skills and experience.
– In periodontal plastic surgery, the choice of procedure is based on the four cardinal principles of any surgery: success, reproducibility, lack of morbidity and economy.
– Basically, the easier the technique the more reproducible it is, since the need for technical skill of the surgeon is reduced.
– The surgeon‘s choice will be based on the confidence he has of his own ability to match the outcomes of the clinical trials.
– Criteria for selection of techniques are:
1. Surgical site free of plaque, calculus, and inflammation
2. Adequate blood supply to the donor site
3. Anatomy of the recipient and donor site (vestibulat depth, width of keratinized gingival,
palatal tissue thickness)
4. Stability of the grafted tissue to the recipient site
5. Minimal trauma to the recipient site
– Several technique-related factors may influence the treatment outcomes:
The flap thickness. Thick gingival tissue eases manipulation, maintains vascularity, and promotes wound healing during and after surgery. Significant moderate correlation
occurred between weighted flap thickness andweightedmean root coverage and weighted complete root coverage (r = 0.646 and 0.454, respectively).
A critical threshold thickness >1.1 mm existed for complete root coverage (P <0.02).
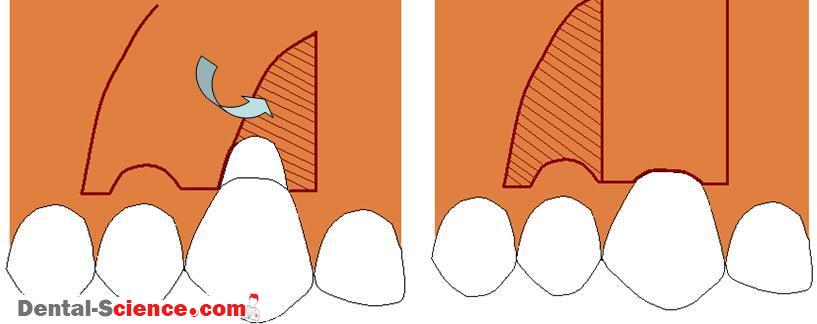
Elimination of flap tension is considered an important factor for the outcome of the
coronally advanced flap procedure.
The position of the gingival margin relative to the cemento-enamel junction after suturing affects the probability of complete root coveragefollowing healing.
– Brouchard et al. revealed several outdated procedures:
– Nonsubmerged grafts are no longer justified in the coverage of recession defects for
aesthetic purposes.
– The procedure is uncomfortable for the patient because of the denuded palatal donor site, and the match with the surrounding tissues is unpredictable.
– The double papilla flap also seems to be a dated technique.
– Use of elaborate sutures is time-consuming. The procedure requires surgeon‘s dexterity.
– Sutures placed over the avascular root surface may lead to postoperative cleft complications that may impair esthetic results.
– Similarly, there seems to be little clinical advantage in using double pedicle flap to cover
connective tissue grafts.
ــــــــــــــــــــ► ⒹⒺⓃⓉⒶⓁ–ⓈⒸⒾⒺⓝⓒⒺ ◄ــــــــــــــــــــ