Root Coverage Procedures
– Surgical procedures used in the treatment of recession defects may basically be classified as:
(1) pedicle soft tissue graft procedures
(2) free soft tissue graft procedures
1. Pedicle Soft Tissue Grafts
– The pedicle graft procedures are, depending on the direct of transfer, grouped as:
(A) rotational flap procedures (e.g. laterally sliding flap, double papilla flap, oblique
rotated flap).
(B) advanced flap procedures (e.g. coronally repositioned flap, semilunar coronally
positioned flap).
– Regenerative procedures are also included within the group of pedicle graft procedures,
i.e. rotational and advanced flap procedures involving the placement of a barrier
membrane between the graft and the root or the application of enamel matrix proteins.
A. Rotational Flaps
– Grupe and Warren introduced the first technique for covering a localized gingival
recession.
– The laterally sliding flap consists of the removal of the collar of the gingiva around the area of recession and elevation of a full-thickness flap on the adjacent tooth.
– This flap is positioned laterally and sutured over the denuded root surface.
– The limitations of the procedure are the amount of the attached tissue and the thickness of the labial bone at the donor site.
– Leaving a thin labial plate exposed on the donor tooth risks recession at this site.
– An laterally positioned pedicle graft cannot be performed unless there is significant gingival lateral to the site of recession.
– A shallow vestibule also may jeopardize outcomes. Although the use of the laterally
positioned pedicle graft provides an ideal color match, it often is inadequate for the
treatment of multiple recessions.
– The Technique is as follows:
– Recipient area. Initially, the recipient area for the laterally moved flap is prepared.
– A reverse bevel incision is made all along the soft tissue margin of the defect.
– After removal of the dissected pocket epithelium, the exposed root surface is thoroughly
curetted.
– Two superficial incisions are then delineating a 3 mm wide recipient area, at the one side of the defect as well as apical to the defect, where the epithelium together with the outer
portion of the connective tissue is removed by sharp dissection.
– The flap design is outlined by two vertical incisions that extended from the horizontal incision to several millimeters apically to the mucogingival junction.
– A horizontal incision is performed either at the gingival or 3 mm apically, following the
marginal gingival contour, thus joining the vertical incisions.
– A beveled linear horizontal incision is performed to optimize the content of keratinized tissue in the flap when the donor site is an edentulous site.
– The flap is elevated as full thickness in the portion adjacent to the recession and as partial thickness in the portion distal to the recession.
– Partial-thickness dissection is continued apically and laterally to obtain passivity of flap
movement and absence of muscle pull or periosteal adhesion.
– The flap is rotated laterally to cover the recession defect completely and extend for
approximately 1 mm coronal to the cemento-enamel junction.
– Careful flap suturing is performed to position and secure the soft tissues over the root surface by means of sling and simple sutures.
– Following removal of the dressing and the sutures, usually after 10-14 days, the patient is
instructed to avoid mechanical tooth cleaning for further 2 weeks, but to use twice daily rinsing with chlorhexidine solution as a means of infection control.
– Several modifications have been described to overcome the problem of dehiscence at the
donor site.
– Staffileno used a split-thickness pedicle flap so as not to denude the adjacent site.
– This approach compromises vascularity and does not preclude bone resorption at the donor site.
– Other modifications of the procedure are the oblique rotated flap, the rotation flap,
the double papilla flap and the trans positioned flap.
– Zucchelli et al. revealed that present data do not seem to indicate the laterally moved flap is an highly predictable and effective root coverage surgical procedure.
– From the studies reviewed, the reported mean percentage of root coverage ranges between 34% and 82% and only Oles et al. (1988) reported data relating the percentage of complete (up to the cemento-enamel junction) root coverage‖ and the range was between 40% and 50%.

B. Advanced Flaps Procedures
– Since the lining mucosa is elastic, a mucosal flap raised beyond the mucogingival junction can be stretched in coronal direction to cover exposed root surfaces.
– The coronally advanced flap procedure has been described by several authors.
– The coronally advanced flap is the first choice surgical technique when there is adequate
keratinized tissue apical to the recession defect.
– Optimum root coverage results, good color blending of the treated area with respect to
adjacent soft tissues, and recuperation of the original morphology of the soft tissues margin can be predictably accomplished using this surgical approach.
– Furthermore, the coronally advanced flap is very effective in treating multiple recession
defects affecting adjacent teeth with obvious advantages for the patient in terms of
esthetics and morbidity.
– Some unfavorable local anatomic conditions may render the coronally advanced flap
contraindicated:
(1) the absence of keratinized tissue apical to the recession defect.
(2) the presence of gingival (-Stillman ‖) cleft extending in alveolar mucosa.
(3) the marginal insertion of frenula.
(4) the presence of deep root structure loss.
(5) presence of a very shallow vestibulum.
– In these situations the clinician should take the soft tissues located laterally to the recession defect into consideration to evaluate the possibility to perform a laterally moved flap.
– The coronally positioned pedicle graft has many advantages over other surgical procedures used to cover exposed roots.
– It does not require a separate surgical site to obtain a graft.
– The tissue utilized will be a perfect color and contour match with the surrounding tissue.
– Additionally, the procedure is simple to perform and does not require a lot of time.
– In aim to evaluate the predictability of the procedure several clinical studies have been
evaluated by Bouchard et al.
– The mean depth of the recession defects treated was 3.7 mm (3.3–4.1mm).
– The mean % of root coverage for advanced flaps was reported to be 77% (55–98), while the % of teeth with complete root coverage was 45% (9-84%).
– More recently, Cairo et al. reviewed the clinical outcomes of the coronally advanced flap on a total of 794 Miller Class I and II gingival recessions in 530 patients from 25 RCTs.
– This systematic review confirms that the coronally advanced flap procedure is a safe and
reliable approach in periodontal plastic surgery and is associated with consistent recession reduction and frequently with complete root coverage.
– The results of meta-analyses showed that only two combinations
(coronally advanced flap + connective tissue graft and coronally advanced flap + enamel matrix derivative) provided better results than coronally advanced flap alone.
– Coronally advanced flap + connective tissue graft resulted in better clinical outcomes for both complete root coverage (OR=2.49) and recession reduction (10.49 mm) compared with
coronally advanced flap, and no other therapy provided better results than coronally
advanced flap + connective tissue graft.
– The combination of coronally advanced flap + enamel matrix derivative was associated with
a higher probability to obtain complete root coverage (OR=3.89) and a higher amount of
recession reduction (0.58 mm) than coronally advanced flap alone.
– A possible benefit following root coverage procedures may be the augmentation of
keratinized tissue.
– This systematic review showed that coronally advanced flap + connective tissue graft was
associated with better clinical outcomes in terms of keratinized tissue gain following
therapy.
– The technique for the coronally advanced flap procedure is:
– The coronally advanced flap is initiated by two horizontal bevelled incisions (3mm in length), mesial and distal to the recession defect located at a distance from the tip of the
anatomical papillae equal to the depth of the recession plus 1 mm.
– Two bevelled oblique, slightly divergent, incisions starting at the end of the two horizontal
incisions and extending to the alveolar mucosa.
– The resulting trapezoidal-shaped flap is elevated with a split–full– split approach in the
coronal–apical direction.
– In order to permit the coronal advancement of the flap, all muscle insertions present in the thickness of the flap are eliminated.
– This is done keeping the blade parallel to the external mucosal surface.
– Coronal mobilization of the flap is considered adequate when the marginal portion of the flap was able to passively reach a level coronal to the CEJ of the tooth with the recession defect.
– In fact, the flap should be stable in its final coronal position even without the sutures.
– The root surface is mechanically treated with the use of curettes.
– It must be considered that only the portion of the root exposure with loss of clinical
attachment (gingival recession1 probeable gingival sulcus/pocket) is instrumented.
– Exposed root surfaces belonging to the area of anatomic bone dehiscence were not
instrumented not to damage connective tissue fibres still inserted in to the root cementum.
– The facial soft tissue of the anatomic inter-dental papillae coronal to the horizontal incisions is disepithelized to create connective tissue beds to which the surgical papillae of the
coronally advanced flap are sutured.
– By moving the flap coronally to reach the tip of the disepitelized anatomical papillae,
the vestibular soft tissue should be positioned 1 mm coronal to the cemento-enamel
junction to account for soft tissue shrinkage.
– The suture of the flap is started with two interrupted periosteal sutures performed at the most apical extension of the vertical releasing incisions; then, it proceeded coronally with other interrupted sutures, each of them directed, from the flap to the adjacent buccal soft tissue, in the apical–coronal direction.
– This is done to facilitate the coronal displacement of the flap and to reduce the tension on the last coronal sling suture.
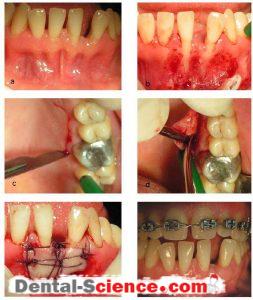
– Coronally advaced flap procedure.
a. A recession defect on the lower canine.
b. Close suturing of the pedicle graft to cover the exposed root surface.
c. Healing outcome 3 months post-operatively.
d. Healing outcome 1 year post-operatively.
– For the treatment of isolated gingival recession, Zucchelli et al. proposed the use of a laterally moved and coronally advanced flap.
– Thereafter, the proposed surgical technique combined the root coverage and esthetic
advantages of the coronally advanced flap with the increase in gingival thickness and in the amount of keratinized tissue associated with the use of the laterally moved flap and
resulted in a very high mean percentage of root coverage (96%) and complete soft tissue root coverage (up to the CEJ) accomplished in 80% of treated cases.
– The main modification of the present surgical technique, with respect to those previously proposed, was the elimination of all muscle insertions in the thickness of the flap to permit the coronal advancement of the laterally moved flap.
– Furthermore, the coronal advancement of the flap allowed the surgical papillae to cover the anatomic papillae which represented the most coronal areas for anchoring the flap and a critical source for vascular exchanges.
– In addition, coronal advancement of the flap beyond the cemento-enamel junction likely compensates for the post-surgical soft tissue contraction, resulting in no exposure of the root surface.
– The different thickness during flap elevation (greater in the central area than in the more
peripheral portions of the flap) represented another aspect of the proposed surgical
technique.
– In a thicker flap the amount of vascularized connective tissue increases and the post-surgical soft tissue contraction decreases.
– Both these factors improve the possibility of accomplishing and maintaining root coverage.
– Another feature of the present surgical technique was the sequence of sutures: the apical
stabilization sutures in the most apical extension and along the releasing incision and the double mattress horizontal suture at the fornix were performed before the marginal sling suture.
– Thus the most marginal portion of the flap was stable in the desired coronal position without disrupting forces acting on it at the time of the final suture.
– Furthermore the double mattress suture reduced lip tension on the marginal portion of the flap during the first healing period and avoided the use of surgical periodontal dressing.
The Semilunar Flap
– The coronally positioned flap may be preferable in situations with multiple recession defects.
– In situations with only shallow defect the semilunar coronally positioned flap described by Tarnow (1986) offers an alternative approach.
– The semilunar coronally repositioned flap has the following advantages:
(1) there is no tension on the flap after coronally repositioning it.
(2) there is no shortening of the vestibule;
(3) the papillae mesial and distal to the toothbeing treated remain cosmetically unchanged.
(4) no sutures are needed because the lack of tension of the tissue being coronally
positioned.
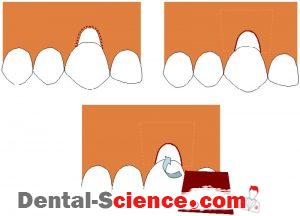
– The technique for the semilunar coronally repositioned is:
– A semilunar incision is placed apically to the recession and at a distance from the soft tissue margin, which should be approximately 3 mm greater than the depth of the recession.
– The outline of the incision should be parallel to the curvature of the gingival margin.
– The incision is extended into the papilla region on each side of the tooth, but care should be taken to secure a collateral blood supply to the pedicle graft.
– A split thickness dissection of the facially located tissue is then made by an intra–crevicular
incision extending apically to the level of the semilunar incision.
– The mid-facial soft tissue graft is coronally repositioned to the level of the cemento-enamel junction and stabilized by light pressure for 5 min.
– No suturing is needed but a light curing dressing is applied for wound protection.
– Despite the lack of tension in the mobilized pedicle, its stability in the more desired coronal position is questionable, as no suturing of the advanced flap portion is indicated.
– This is of particular concern when the procedure is considered for teeth with highly scalloped gingival margins, where coronally manipulating the tissue could be more demanding.
– The semilunar flap is a modification of a technique described in the late 1960s for incisally
repositioning the gingival tissues to address recession defects on labial surfaces of maxillary cuspids.
– In a in a split-mouth design the outcome of gingival recession therapy using subepithelial
connective tissue graft or the semilunar coronally positioned flap procedure was evaluated by Bittencourt et al.
– No statistically significant differences were observed between groups in any of the clinical
parameters at baseline.
– Recession height, recession width, width of keratinized tissue, thickness of keratinized tissue, probing depth, and clinical attachment level were measured at baseline and 6 months
post-surgery.
– In the subepithelial connective tissue graft group, recession height decreased from 2.20 ± 0.56 mm to 0.21 ± 0.25 mm, corresponding to a mean root coverage of 90.95% ± 11.46%.
– In the semilunar coronally positioned flap group, recession height decreased from 2.15 ± 0.59 mm to 0.10 ± 0.19 mm, corresponding to a mean root coverage of 96.10% ± 7.69. Complete root coverage was accomplished in 52.94% of the treated cases in the subepithelial
connective tissue graft group and in 76.47% in the semilunar coronally positioned flap group.
– After 30 months, the mean percentages of root coverage were 89.25% and 96.83% for the semilunar coronally positioned flap and subepithelial connective tissue graft groups,
respectively.
– Complete root coverage at the final observation was achieved in 58.82% of the treated cases in the semilunar coronally positioned flap group and in 88.24% of the patients in the
subepithelial connective tissue graft group.
– The comparison between 6 and 30 months showed that two patients in the subepithelial
connective tissue graft group gained attachment and achieved complete root coverage; this only occurred in one patient in the semilunar coronally positioned flap group.
– The subepithelial connective tissue graft group maintained a statistically significant increase in thickness of keratinized tissue (P<0.05) at 30 months.
– At this time, there were no significant differences between the two groups with regard to
recession height, recession width, width of keratinized tissue, thickness of keratinized
tissue, probing depth and clinical attachment level.
– With regard to esthetic improvement, after 30 months, patients in semilunar coronally
positioned flap and subepithelial connective tissue graft groups were generally satisfied with both procedures (82.3% and 100%, respectively).
– Although they presented similar good results, more patients preferred, based on esthetics achieved, treatment with subepithelial connective tissue graft.
– This can be explained by the higher percentage of complete RC and the absence of
hypertrophic scars or fibrosis in this group, whereas in the semilunar coronally positioned flap group, seven patients complained about the presence of hypertrophic scars, although they were not visible while smiling.
– The modified semilunar coronally advanced flap for the correction of gingival recession
present on adjacent teeth was described by Haghigha.
– Semilunar incisions were made apical to the recession defects, starting within mucosa and
extended mesio-distally, arching more coronally to terminate apical to the papillae mesial and distal to the teeth exhibiting the defects.
– The papilla between the teeth with recession was coronally advanced after a split thickness dissection and sutured more coronally, over the deepithelialized portion of the original
papilla.
– This technique provides better control over flap repositioning than previously described
semilunar coronally advanced flaps and reduces the likelihood of apical tissue retraction when attempting root coverage on two adjacent teeth.
– This is particularly of value for highly scalloped gingival margins where coronal manipulation and stability are difficult.
– As described with the original semilunar flap procedure, adequate thickness and width of
keratinized tissue apical to the recession defect are required.
– In cases exhibiting a thin-tissue biotype, tissue augmentation either before or at the time of the corrective surgery is advocated.
– Therefore, the technique is of value in the correction of residual recession defects on two
adjacent teeth where previous attempts at coverage using soft tissue autografts have been made.
C. Pedicle Soft Tissue Graft Procedures Combined with a Barrier Membrane
– Regeneration is defined as ―a reproduction or reconstitution of a lost or injured part.
– It is, therefore, the biologic process by which the architecture and function of lost tissues are completely restored.
– This implies regeneration of the tooth‘s supporting tissues, including alveolar bone,
periodontal ligament, and cementum.
– Many studies have attempted to achieve regeneration, but success rates have varied from minimal or partial regeneration to almost complete regeneration.
– The use of GTR has been suggested for treatment of recession.
– In considering healing dynamics of the root-gingiva interface, regeneration may be influenced by factors related to morphological characteristics of the recession defect, the surgical
manipulation as well as traumatic events during the early healing phase.
– The lack of a horizontal and angular component of the associated bone defect facilitates close proximity of the exposed root surface to proliferating cells assumed necessary for
regeneration of the site.
– It is reasonable to assume that the deeper and narrower the defect, the greater the
periodontal regeneration occurring away from disturbing environmental factors.
– Factors such as tooth location, vestibular depth, and muscular and frenum insertions may
affect wound stability once a pedicle flap is advanced onto an exposed root.
– Flap management, suturing technique, and post-surgery wound protection should be adapted to the peculiar anatomic conditions of the gingival recession defect to optimize wound
stabilization.
– The last decade has seen an increasing number of clinical reports on guided tissue
regeneration (GTR) for reconstruction of gingival recession defects.
– Danesh-Meyer and Wikesjo evaluated the efficacy of GTR procedures to provide root
coverage in gingival recession defects and reviewed studies and case-series using
non resorbable and bio resorbable membranes, studies comparing GTR to the subepithelial connective tissue graft procedure, and histologic reports of healing following GTR,
published in the English language from 1985 to 2000.
– Root coverage among the studies using nonresorbable membranes averaged 3.5±0.7 mm.
– Clinical attachment level gain averaged 4.0±0.9 mm.
– Importantly, probing depths in the augmented sites remained shallow following the GTR
protocol.
– Limited mean increase in keratinized gingiva (0.6±0.8 mm) was observed among studies using non-resorbable membranes.
– Keratinized gingivas ranged from 1.0 to 1.9 mm pre-treatment compared to 0.5 to 6.2 mm post-treatment.
– A majority of studies reviewed reporting observations of membrane exposure,
this compromise of the efficacy of GTR is an important consideration in the general utility of this technology for gingival recession defects.
– To eliminate the need for a second surgical procedure to remove a nonresorbable
membrane, the use of various bioabsorbable materials has been proposed.
– The majority of studies evaluating bioresorbable membranes for treatment of gingival
recession defects are case studies typically involving only few subjects.
– The variety of biomaterials complicates any comparisons between studies as the materials may differ in physical properties including biocompatibility, cell exclusion, clinical
manageability, tissue integration, space provision, space maintenance, and bioresorbtion, all of which may inffluence their ultimate relevance as GTR devices.
– Root coverage among the studies using bioresorbable membranes averaged 2.8±1.2 mm.
– CAL gain averaged 2.5±1.3 mm.
– As observed for nonresorbable membranes, probing depths remained shallow following the GTR protocol.
– Bioresorbable membranes appear less effective than the nonresorbable membrane
technology in more limited gingival recession defects, however this relative deficiency
appears compensated in advanced defects.
– As observed for the nonresorbable membrane technology, keratinized gingiva increases slightly following GTR using bioresorbable membranes.
– This increase, however, appears to be smaller than for nonresorbable membranes, several studies actually reporting no effect or decreased keratinized gingival post-treatment.
– Studies comparing GTR and subepithelial connective tissue graft suggest that both protocols offer means of obtaining root coverage of gingival recession defects.
– It appears, however, that the subepithelial connective tissue graft protocol provides
improved root coverage over that observed following GTR.
– The subepithelial connective tissue graft protocol also results in a substantially increased KG compared to only incremental improvements following GTR.
– A possible explanation for these observations may be the occurrence of membrane exposures and ensuing compromised wound healing following GTR.
– In a meta-analysis on forty studies, Al-Hamdan et al. revealead that guided tissue
regeneration-based root coverage resulted in an average of 74% recession depth reduction, 41% complete root coverage, 3 mm CAL gain, and 1 mm keratinized gingival gain.
– Both guided tissue regeneration-based root coverage and conventional mucogingival surgery produced significant (P<0.05) improvement compared to baseline measurements.
– Compared to guided tissue regeneration-based root coverage, conventional mucogingival surgery resulted in significantly (P<0.05) increased keratinized gingiva (2.1 mm vs. 1.1 mm), root coverage (81% vs. 74%), and percentage of defects with complete root coverage (55% vs. 41 %).
– Use of absorbable membranes, root conditioning, shallow pretreatment recession (< 4 mm), and corporate sponsorship all resulted in significantly (P<0.05) improved percentages of sites with complete root coverage but had no effect on other parameters.
D. Pedicle Soft Tissue Graft Procedures Combined with Enamel Matrix Proteins
– Enamel matrix derivative, harvested from
embryonic porcine teeth, has been extensively studied in animals and humans and has been also proposed to be used in the treatment of root coverage.
– The technique as described by Berlucchi et al. is as follows:
– An intrasulcular incision is made, under local anesthesia, on the buccal aspect of the gingiva.
– The incision is extended horizontally up to one or two teeth mesially and distally to the tooth involved in order to mobilize the flap, avoiding vertical releasing incisions to preserve as much blood supply as possible.
– A full thickness flap was then elevated beyond the mucogingival junction; next, a partial
thickness flap is elevated in order to mobilize the flap, ensuring a passive coronal
adaptation 1 to 2 mm above the cemento-enamel junction.
– Afterwards, the papillae adjacent to the involved tooth were de-epithelialized and a sling
suture is placed, but left untied, mesially and distally to the recession.
– Then, the root surface is conditioned with an ethylenediamine-tetraacetic acid (EDTA) gel 24% for 2 minutes, in accordance with the manufacturer‘s indication, and rinsed with saline solution.
– EMD is applied on the conditioned root surface and the suture is tied, positioning the flap
1 to 2 mm above the cemento-enamel junction.
– Single or sling sutures are used to secure the other papillae.
– Cheng et al. (2007) reviewed coronally positioned flap, coronally positioned flap + chemical root surface conditioning, or coronally positioned flap + enamel matrix derivative (EMD)
for the treatment of Miller class I and II gingival recession.
– Clinically, the present analysis demonstrated that all three groups are useful in treating
Miller‘s class I and II recession defects.
– All three groups achieved considerable root coverage and gains in clinical attachment, and maintained the amount of keratinized tissue and shallow probing pocket depths.
– The application of EMD to denuded root surfaces treated with the coronally positioned flap procedure significantly increased the percentage of root coverage and the attachment level compared with coronally positioned flap alone and the coronallypositioned flap + chemical root surface conditioning procedure.
– In thepresent review, the coronally positioned flap and coronally positioned flap + chemical root surface conditioning groups resulted in root coverage percentage values ranging from 55 to 75%.
– The mean root coverage percentage of coronally positioned flap + EMD-treated sites ranged from 71.7 to 95.1%.
– The average root coverage of coronally positioned flap plus EMD amounted to 84.33 ± 7.72% after 6 mo and 84.42 ± 8.75% at 12 mo. The outcome of coronally positioned flap + EMD was better than coronally positioned flap alone after 6 months (74.12 ± 15.80%) and 12 months (79.00 ± 0.00%).
– The amount of root coverage obtained was quite stable between 6 and 12 mo in the
coronally positioned flap + EMD group for root coverage.
– This suggests that root coverage procedures in the coronally positioned flap alone and
coronally positioned flap + chemical root surface conditioning procedures were
unpredictable.
– They became more predictable when the coronally positioned flap procedure was improved by the modification of adding EMD.
2. Free Soft Tissue Grafts
– The autogenous free soft tissue graft procedures may be performed as:
(A) an epithelized graft.
(B) a subepithelial connective tissue graft (non-epithelized graft).
both usually taken from the area of the masticatory mucosa in the palate.
A. Epithelialized Soft Tissue Graft
– A free soft tissue graft of masticatory mucosa is usually selected when there is no acceptable donor tissue present in the area adjacent to the recession defect or when a thicker marginal tissue is desirable.
– The procedure can be used for the treatment of a single tooth as well as for groups of teeth.
– The graft can be nonsubmerged: that is, placed on the surface of the recipient bed;
or submerged, when the graft is completely or partially covered by flap.
– The epithelialized soft tissue graft is commonly named free gingival graft.
– The procedure can be performed either as a one-step technique, in which the graft is placed directly over the root surface either as a two-step surgical technique, where
an epithelialized free soft tissue graft is placed apical to the recession and following healing is coronally positioned over the denuded root.
– The characteristics of the incision at the recipient site are important as means to optimize blood supply to the graft.
– Horizontal and vertical incisions should be made at a 900 angle, in a butt joint fashion.
– Beveled incisions may result in a tendency for the graft to slide over the incision lines with
resultant dead space between the graft and the graft bed and, therefore, blood supply may be compromised.
– The vertical incisions in the recipient site should be placed close to the line angles of the
adjacent teeth in order for wide surgical papillae to be present and consequently facilitate suturing and maximize blood supply from the papillary areas.
– As a matter of fact, graft thickness should be considered as an important criteria and should be controlled carefully.
– The grafts used should be approximately 0.8 to 1.5 mm in thickness to assure that there is an adequate connective tissue component.
– However, deep wounds at the donor site may be created while receiving a transplant tissue from the palatal donor site.
– This donor region may be a source of arterial injury.
– In addition, an unaesthetic bulky tissue profile may also occur at the recipient site.
– On the other hand, very thin grafts (0.5 to 0.6 mm thickness) demonstrate a better
color blending with that of the neighboring tissues.
– After utilization of a free soft tissue graft, the vestibular depth of the recipient area may be diminished by the contraction of the wound and by the reinsertion of the muscle fibers in postoperative stage.
– Different clinical studies presented a broad range of shrinkage percentages
between 12% and 48%.
– Silva et al. (2010) sought to determine the effect of smoking on free soft tissue graft
donor-site healing.
– A significantly lower proportion of smokers exhibited immediate bleeding after graft
harvesting compared to non-smokers.
– Non-smokers had almost twice as long median time to achieve hemostasis compared to smokers in However, at 15 days 92% of non smokers sites and only 20% of smokers
demonstrated complete epithelialization.
– At 30 days after the surgery, all sites in both groups demonstrated complete epithelialization.
– The free gingival graft used for root coverage presents distinct advantages over other surgical techniques, but also has its limitations.
– With appropriate case selection, this technique is predictable in achieving complete root
coverage.
– The free gingival graft appears to be the best treatment alternative in areas where gingival recession is combined with lack of adequate vestibular depth and for teeth requiring root coverage prior to receiving a restoration with subgingival margins.
– An overview of studies on the effect of the free soft tissue graft as a means for root coverage was performed by Wennström.
– The mean initial depth of the recessions included was 2.1 mm to 5.1 mm.
– The mean percent root coverage obtained with the free soft tissue graft procedure varied
between 11% and 87%, with the greatest success in narrow and shallow defects.
– Considering the number of teeth treated in each study, the calculated average percentage of root coverage studies is 72%.
– The predictability of complete root coverage ranged from 0% to 90%, with an average of 57%.
– The limitations and disadvantages of the free gingival graft for root coverage include
increased discomfort and potential for postoperative bleeding from the donor area by
virtue of a large wound that heals by secondary intention.
– The palatal surgical wound heals with secondary intention within 2–4weeks due to the
removal of the epithelial layer of the palatal mucosa.
– Compared with other soft tissue techniques for root coverage, the free gingival graft results in an unpredictable color match between the grafted tissue and adjacent gingival tissues.
– Grafted tissue with a lighter color than desired may persist for long periods of time after the initial healing.
– Finally, this procedure is technique sensitive and attention to the details involved in the
execution of the surgery is crucial in order to achieve a successful outcome.
B. Connective Tissue Graft
– The technique utilizing a subepithelial soft tissue graft, i.e. the connective tissue, involve the placement of the graft directly over the exposed root and the mobilization of a mucosal flap coronally or laterally for coverage of the graft.
– The most common indications for the CTG are esthetic demands from the patients, Miller Class I and II recession, dental hypersensitivity because of exposed cementoenamel
junction and the necessity to augment a narrow band of keratinized gingival tissue.
– The relative contraindications that may limit the results of the connective tissue autograft are heavy smoking, impaired healing response from the patient, Miller Class II I or IV recession, or the existence of an extremely thin periodontium that would limit the amount of donor tissue.
– The tehnique of connective tissue graft covered by a coronally advanced flap is as follows:
– A horizontal incision is first made in the facial surface of the interdental tissue on each side of the teeth to be treated. The incision should be placed just coronal to the intended level of root coverage. Care should be taken not to decrease the height of the papilla. Subsequently, starting from the line of incision in the interdental area at the mesial and distal termination of the surgical area, two divergent, vertical incisions are placed and extended well beyond the mucogingival line.
– A split thickness flap is then prepared by sharp dissection and elevated to such an extent that it can be coronally repositioned at the level of the cementoenamel junction
without tension.
– A subepithelial connective tissue graft of masticatory mucosa is harvested on the palatal
aspect of the maxillary premolars (or from retromolar pad) by the use of a-trap door
approach. Before incisions are placed, the available thickness of the mucosa is estimated by the use of the type of the syringe.
A horizontal incision, perpendicular to the underlying bone surface, is made approximately 3mm apical to the soft tissue margin in the premolar region.
The mesiodiostal extension of the incision is determined by the graft size required.
To facilitate the removal of the graft, a vertical releasing incision can be made at the mesial termination of the primary incision. An incision is then placed from the line of the first incision and directed apically to perform a split incision of the palatal mucosa.
A small periosteal elevator is used to release the connective tissue graft.
Sutures may be placed in the graft before it is released completely free from the donor area to facilitate is placement at the recipient site.
– The graft is immediately placed in the recipient site and secured in position with interrupted sutures. The mucosal flap is then sutured to cover the connective tissue graft. Interrupted sutures are placed in the papilla region as well as along the wound of the vertical incisions. It is recommended to place a surgical dressing for protection of the area during the first week of healing.
– It has been showed that the clinical outcome of this surgical method is not affected by orientation of connective tissue graft nor by the presence of the epithelial collar.
– Bouchard et al. (2001) performed an evaluation of 16 studies on the effect of free
connective tissue grafts in the treatment of recession defects.
– The maximum length of the selected studies was 18 months.
– The mean initial depth of the treated recessions was 3.9 mm (3.3-4.9mm) for submerged grafts followed by rotational flaps the mean % of root coverage (range) was 83% (70-97). When considering the submerged grafts followed by coronally positioned flap at a mean
initial depth of the treated recessions of 4.0 mm (3.0-5.6 mm), the mean % of root coverage (range) was 82% (52-99).
– Chambrone et al. (2008) evaluated the effectiveness of subepithelial connective tissue grafts over other techniques when used in the treatment of recession defects, in terms of changes in clinical outcomes, occurrence of adverse effects, aesthetic condition and patient‘s
satisfaction.
– The results indicated a statistically significant greater reduction in gingival recession for
subepithelial connective tissue grafts, when compared to acellular dermal matrix graft (Weighted mean difference -0.63mm; 95% CI: -1.26, 0.00) and guided tissue regeneration with resorbable membranes(Weighted mean difference -0.41mm; 95% CI: -0.62, -0.20).
– For clinical attachment level changes, differences in CAL gain between all groups were not significant.
– For changes in the width of keratinized tissue, the results showed a statistically significant gain in the width of keratinized tissue for subepithelial connective tissue grafts when
compared to guided tissue regeneration with resorbable membranes (Weighted mean
difference -1.46mm; 95% CI: -2.12, -0.81), guided tissue regeneration with non-resorbable membranes (Weighted mean difference -1.82mm; 95% CI: -3.28, -0.35) and guided tissue regeneration with resorbable membranes associated to bone substitutes (Weighted mean difference -2.10mm; 95% CI: -2.51, -1.69). The percentages of compete root coverage and mean root coverage showed markedly variation. Procedures of subepithelial connective
tissue grafts have given 8.6% – 96.1% complete root coverage and 64.5% – 97.3% mean root coverage.
– Overall comparisons allowed the authors to consider subepithelial connective tissue graft as the ―gold standard‖ procedure in the treatment of recession-type defects.
– Subepithelial connective tissue grafts have been showed to be statistically superior to guided tissue regenerationwith resorbable membranes in achieving root coverage.
– Acellular dermal matrix grafts were proposed as an alternative in cases where subepithelial connective tissue grafts harvested from the palate are not sufficient to cover a recession area.
The “Envelope” Technique
– Several modifications have been developed in managing the connective tissue (CT) graft.
– Raetzke (1985) demonstrated an envelope‘ technique with no releasing incisions to secure the donor CT into an envelope created around the denuded root surface of a single gingival recession defect.
– The sulcular epithelium of the affected tooth is removed and the exposed root is thoroughly scaled and planed followed by treatment with citric acid.
– A partial thickness envelope is created in the tissues surrounding the recession.
– A graft twice the width of the area of recession is placed into the envelope, completely
covering the exposed root.
– Finger pressure is then applied to stabilize the graft until hemostasis is achieved.
– Tissue adhesive is used to keep the graft in place rather than sutures.
– Cordioli et al. (2001) evaluate root coverage and mucogingival changes 1 to 1.5 years
following treatment of Miller’s Class I and II recession defects using 2 variants of the
subepithelial connective tissue graft procedure.
– Results showed a mean root coverage percentage of 89.6 ± 15% for the envelope technique group and 94.7 ± 11.4% for the coronally positioned flap combined with connective tissue graft group; the difference between groups was statistically insignificant (P>0.05).
– Mean keratinized tissue increased significantly from 1.4 ± 1.1 mm pre surgery to 4.5 ± 1.1 mm post surgery for the envelope technique group while a minor increase in KT was observed in the coronally positioned flap combined with connective tissue graft group (2 ± 1.5 mm
presurgery versus 2.7 ± 1.6 mm postsurgery).
– For an mean initial recession depth of 2.9 mm (2.5-3.4), an mean % root coverage of 83%
(80-87) has been reported.
– Among four studies reviewed, the % teeth with complete root coverage was 53 (42–62).
– The key to the envelope flap is that it preserves the lateral and apical blood supply of the flap by eliminating vertical release incisions.
– This technique minimizes surgical trauma to the recipient bed and provides good healing and excellent esthetic results.
– Among various connective tissue graft procedures, it is the last conducive to complete
coverage of the defect by the overlying tissue, because of the manner in which the recipient bed is prepared.
– In general, this surgical method provided excellent root coverage and an increased amount of keratinized gingiva.
– Vergara and Caffesse reported that thecomplete root coverage mean was 85%, 65%, and 16% for recession Class I, II, and IV, respectively.
The “Tunnel” Technique
– The treatment of multiple adjacent gingival recessions with a tunnel subepithelial connective tissue graft has been proposed.
– The surgical procedure involves a connective tissue graft placed in a multienvelope recipient bed (tunnel).
– This tunnel is made of a supraperiosteal bed under a pedicle flap without any external
incisions.
– A connective tissue graft is then placed and secured through this tunnel, covering the
adjacent exposed roots.
– The specific indications for surgical intervention with the tunnel CTG include multiple
adjacent recessions, situations in which very early healing is needed for esthetic demands, or a need to reduce the number of surgical interventions.
– Tözüm et al. compared the efficiency of two different modified tunnel technique with the Langer and Langer, in Miller Class I and II gingival recessions.
– Langer and Langer described the root coverage technique in which the overlying partial
thickness flap with two vertical incisions covers the transplanted connective tissue graft.
– Both techniques demonstrated highly predictable root coverage and attachment gain at 6 months post-surgery, but better results were obtained for the tunnel technique for root coverage and attachment gain.
– A mean root coverage of 3.36 ± 0.17 mm and 3.93 ± 0.27 mm attachment gain were noted in the tunnel group compared to the Langer and Langer group, where a mean root coverage of 2.56 ± 0.19 mm (P<0.005) and 2.44 ± 0.34 mm (P<0.005) attachment gain were achieved.
– The percentage of root coverage was 96.4% and 75.5% and attachment gain was 77.1% and 56.4% in the tunnel and Langer and Langer groups, respectively.
– Subepithelial connective tissue grafts with modified tunnel approach have showed also
long-term stability of the results.
– It was reported a mean root coverage was 95% and 92.2% at eight months and 36 months postsurgery, respectively.
– These differences were statistically significant compared to the baseline.
– The mean gain in attachment was 3.79 mm, and the mean root coverage was 3.14 mm after 36 months.
– The tunnel technique offers successful clinical results for both patients and clinicians, as preservation of the interdental papillae reduce the trauma at the recipient site and improve early esthetic results.
ــــــــــــــــــــ► ⒹⒺⓃⓉⒶⓁ–ⓈⒸⒾⒺⓝⓒⒺ ◄ــــــــــــــــــــ