Gingival Biotypes
– The gingival morphology of the maxillary anterior region plays an important role in
determining the final esthetic outcome.
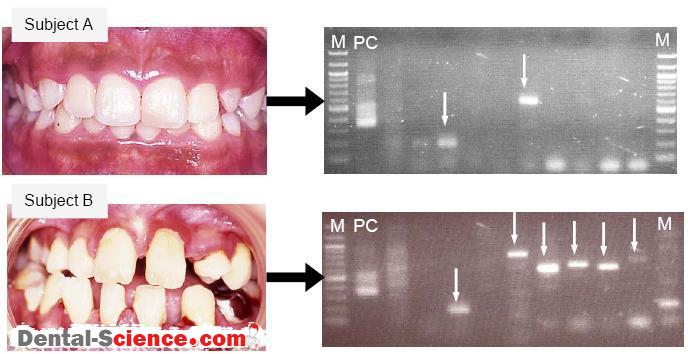
– Clinical observations have led clinicians to identify two basic human periodontal forms.
– The more prevalent, the thick flat type, occurs in over 85% of the patient population; the other, the thin scalloped type, occurs in less than 15% of cases.
– In the thick flat type there is this normal rise and fall of the gingival and bone, but there is not a great disparity between the direct facial and that found interproximally.
– The gingiva is thick or dense and is fibrotic in nature.
– Usually this type of periodontiurn has, quantitatively and qualitatively, adequate amounts of attached masticatory mucosa.
– The teeth found in the thick flat periodontium are usually characterized by being more
bulbous and square in form.
– Contact areas are located more apically and usually are broad inciso gingivally and
faciolingually.
– The interproximal papillae filling the space between the teeth terminate at the contact areas, hence, a flat periodontium.
– When irritated by tooth preparation, impression procedures, extraction, or other clinical techniques, this periodontium usually reacts with inflammation, followed by migration of the junctional epithelium apically, with resultant periodontal pocket formation
or redundant tissue.
– Predicable soft and hard tissue contour after healing following surgery and minimal ridge
resorption occurs after extractions.
– The thin scalloped type of periodontium, on the other hand, is distinguished by a pronounced disparity between the height on the direct facial and that found interproximally.
– The underlying bone is usually thin on the facial with dehiscences and fenestrations
commonly found.
– Usually there is less attached masticatory mucosa, from both quantitative and qualitative
perspectives.
– In the thin scalloped periodontium, the tooth form is usually more subtle and somewhat
triangular.
– Contact areas are located more incisally and are small incisogingivally and faciolingually.
– The cervical convexity is less prominent.
– Since the contact areas are located more incisally, the interproximal papilla is also positioned more incisally, hence, the scalloped form.
– Excessive irritation of this type of periodontium usually leads to recession both facially and interproximally.
– In this gingival biotype after surgery it is difficult to predict where tissue will heal and stabilize and extensive ridge resorption in the apical and lingual direction usually occurs after
extractions.
– Many methods have been proposed to measure gingival tissue thickness:
– Direct measurements.
– Probe transparency. This evaluation was based on the transparancy of the periodontal probe through the gingival margin while probing the sulcus at the midfacial aspect of the examined tooth. If the outline of the underlying periodontal probe could be seen through the gingival, it was categorized as thin; if not, it was categorized as thick.
– Ultrasonic devices.
– Cone-beam computer tomography (CBCT).
– The identification of the gingival biotype may be important in clinical practice since
differences in gingival and osseous architecture have been shown to exhibit a significant
impact on the outcomes of periodontal therapy, root coverage procedures, orthodontic therapy and implants esthetics.
– Hwang and Wang (2006) reviewed the current literature to verify the presence of any
association between gingival thickness and root coverage outcomes.
– Fifteen investigations were included.
– All of these reported at least 0.7mm of flap thickness, although measurement locations
varied.
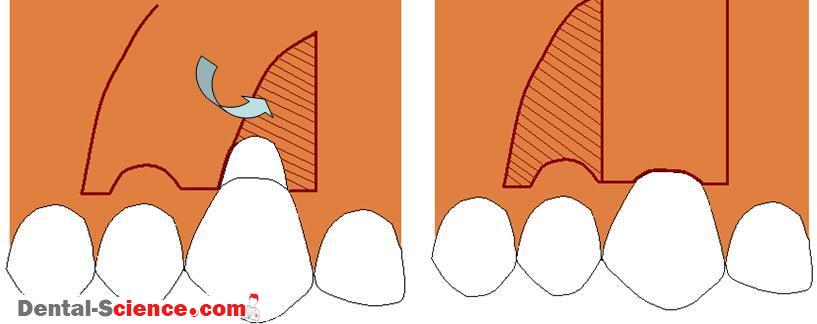
– Treatment modalities included coronally advanced flap, connective tissue graft, and guided tissue regeneration with and without adjuncts.
– A significant moderate correlation occurred between weighted flap thickness and weighted mean root coverage and weighted complete root coverage (r = 0.646 and 0.454,
respectively; weighted mean of gingival thickness accounted for 41.7% of variability in weighted mean root coverage results and a lesser proportion (20.7%) in weighted complete root coverage.
– The paradigm shift proposed by Kao et al. (2008) was that by taking into consideration the gingival tissue biotype during treatment planning, more appropriate strategies for
periodontal management may be developed, resulting in more predictable treatment
outcomes.
ــــــــــــــــــــ► ⒹⒺⓃⓉⒶⓁ–ⓈⒸⒾⒺⓝⓒⒺ ◄ــــــــــــــــــــ